The convergence of Type 2 Diabetes Mellitus (T2DM) and Chronic Kidney Disease (CKD) – often termed diabetic kidney disease (DKD) – represents a devastating clinical duet. T2DM, characterized by insulin resistance and hyperglycemia, inflicts gradual damage on the delicate filtering units of the kidneys (nephrons). This damage, driven by metabolic dysregulation, hypertension, and chronic inflammation, manifests as CKD, where kidney function progressively declines. Patients endure a spectrum of burdensome symptoms: debilitating fatigue, persistent fluid retention leading to edema, poorly controlled hypertension, electrolyte imbalances, and ultimately, the looming threat of kidney failure. Traditional management hinges on stringent glycemic control (metformin, SGLT2 inhibitors, GLP-1 RAs), blood pressure management (ACEi/ARBs), and lifestyle modifications. While these slow progressions, they cannot halt it or regenerate lost function, leaving dialysis or transplantation as eventual, often unavoidable, endpoints.
Beyond Palliation: The Dawn of Regenerative Medicine
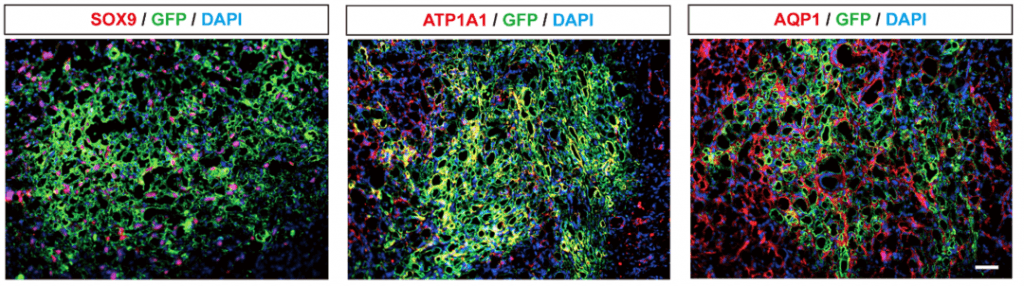
Enter autologous renal progenitor cell therapy, exemplified by products like Gemiracel’s REGEND003. This innovative approach harvests a patient’s own (autologous) renal progenitor cells (RPCs) – precursor cells residing within the kidney with inherent regenerative potential. Isolated and expanded ex vivo, these cells are reintroduced into the patient’s kidneys. The therapeutic rationale is profound: RPCs possess the remarkable ability to differentiate into multiple renal cell types (podocytes, tubular epithelial cells) and secrete a potent cocktail of trophic factors. This dual action promotes tissue regeneration by replacing damaged cells and stimulating endogenous repair mechanisms, while simultaneously modulating the local inflammatory and fibrotic microenvironment that drives CKD progression. Crucially, by targeting the underlying pathology with the patient’s own cells, REGEND003 aims for true functional reconstruction, potentially restoring filtration capacity lost in DKD, an outcome unattainable with conventional drugs.
Precision Delivery: Rilparencel vs. REGEND003
Another contender in this space is Rilparencel, utilizing targeted intrarenal delivery. While both Rilparencel and REGEND003 represent cutting-edge cell therapies for CKD, their core strategies differ significantly:
- REGEND003 (Gemiracel): Utilizes autologous renal progenitor cells (RPCs) sourced directly from the patient’s kidney tissue. These cells are intrinsically programmed for kidney-specific repair and regeneration. The therapy leverages the cells’ natural homing ability and paracrine signaling to orchestrate tissue restoration.
- Rilparencel: Typically employs allogeneic mesenchymal stem cells (MSCs) derived from donor sources (e.g., bone marrow). Its key innovation is the targeted intrarenal delivery method, using specialized catheters to precisely infuse cells directly into the renal arteries or parenchyma, aiming to maximize local engraftment and minimize systemic dispersion.
Advantages & Distinctions:
REGEND003’s use of autologous RPCs potentially offers superior tissue-specificity and avoids immune rejection concerns inherent to allogeneic approaches like Rilparencel. RPCs are developmentally primed for renal repair, potentially offering a more direct path to reconstructing functional nephrons. Rilparencel’s targeted delivery is a significant technological advantage for ensuring cell localization, which could be beneficial regardless of cell type, and its allogeneic nature provides an “off-the-shelf” logistical benefit. The critical question remains whether the inherent regenerative potential of kidney-specific progenitors (REGEND003) outweighs the delivery precision and convenience of allogeneic MSCs (Rilparencel) in achieving durable functional recovery.
A Global Imperative and the Promise of Regeneration
The global burden of CKD is staggering and escalating, fueled by rising diabetes and hypertension prevalence. Current estimates suggest over 800 million individuals live with CKD, with DKD being the leading cause of end-stage renal disease (ESRD) worldwide. This epidemic places an unsustainable strain on healthcare systems, underscored by the immense cost and reduced quality of life associated with dialysis and transplantation.
The emergence of therapies like REGEND003 and Rilparencel signals a paradigm shift. Moving beyond merely slowing decline, they aim for true functional restoration. REGEND003, by harnessing the patient’s own kidney-specific repair cells, represents a particularly elegant biological strategy. Its demonstrated potential to stimulate de novo tissue generation and mitigate fibrosis offers hope not just for DKD, but for a broad spectrum of CKD etiologies characterized by irreversible structural damage – including hypertensive nephrosclerosis, certain glomerulonephritides, and even post-acute kidney injury fibrosis. The vision is a future where regenerative medicine provides a viable alternative to organ replacement, fundamentally altering the trajectory for millions living under the shadow of kidney failure.
While challenges in standardization, scalability, and long-term efficacy data remain, the trajectory of renal progenitor cell therapy is undeniably promising. REGEND003 exemplifies a powerful approach leveraging intrinsic repair mechanisms. Its development, alongside innovations like Rilparencel’s delivery, illuminates a path towards transforming CKD management from chronic palliation to genuine restoration, offering a beacon of hope against a relentlessly growing global health challenge.