Hematopoietic stem cells are like the body’s main builders for blood. These special cells are found in the bone marrow. They make all kinds of blood cells, like red cells, white cells, and platelets. Every mature blood cell in the body comes from hematopoietic stem cells. If someone has a serious blood disease, doctors might use transplantation. In transplantation, healthy hematopoietic stem cells take the place of damaged ones. Transplantation gives people hope. It can help both kids and adults. Transplantation saves lives. It works because of hematopoietic stem cells. Transplantation gives people another chance. It uses the special power of hematopoietic stem cells.
Hematopoietic Stem Cells
What They Are
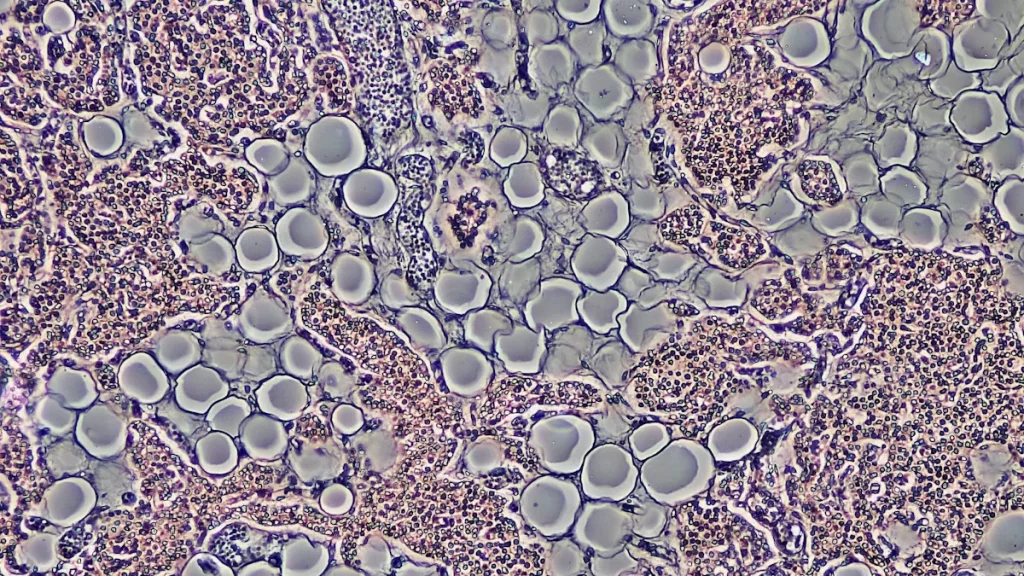
Hematopoietic stem cells are the base of the hematopoietic system. These cells are rare and very important. They can make every kind of blood cell in the body. Scientists call this special power pluripotency. Hematopoietic stem cells create red blood cells, white blood cells, and platelets. They can also make more copies of themselves. This helps the hematopoietic system work for a person’s whole life. Hematopoietic progenitor cells come from these stem cells. They help the cells change into different blood cells. This process is called differentiation. Differentiation lets each cell become a certain type of blood cell.
Where They Are Found
Most hematopoietic stem cells are in the bone marrow. The bone marrow is their main home after birth. When a baby is growing, these cells first show up in the aorta-gonad-mesonephros area. Later, they move to the liver. Then they settle in the bone marrow. In healthy grown-ups, the bone marrow is still their main place. Some hematopoietic stem cells are also in peripheral blood and umbilical cord blood. Doctors collect peripheral blood progenitor cells and umbilical cord blood. These are used to help people who need hematopoietic stem cell transplants.
Key Properties
Hematopoietic stem cells are special because of what they can do.
- They can copy themselves and also become different blood cells.
- Self-renewal happens when the cells divide and make more stem cells.
- Differentiation lets them turn into red cells, white cells, or platelets.
- Most of these cells stay quiet and do not divide all the time.
- The bone marrow niche sends signals to control what the cells do.
- These cells can move from the bone marrow to the blood.
- They can handle stress, like irradiation, and can help fix damaged hematopoietic tissue after a transplant.
Note: The right balance between self-renewal and differentiation keeps the hematopoietic system healthy and ready to help the body.
How Hematopoietic Stem Cells Work
Blood Cell Production
Hematopoietic stem cells are very important in the hematopoietic system. Most of these cells are found in the bone marrow. They make more stem cells by self-renewal. They also make new blood cells by differentiation. The body must replace old or damaged blood cells every day. Hematopoietic stem cells help by making billions of new cells daily. The bone marrow is where this happens.
- Grown-ups make about 400 to 500 billion new blood cells each day.
- Hematopoietic stem cells in the bone marrow are the main source for this.
- These cells use self-renewal and differentiation to keep blood cell numbers steady.
Differentiation follows certain steps. Each blood cell type comes from hematopoietic stem cells in a special way:
| Blood Cell Type | Differentiation Pathway from HSCs | Location of Maturation |
|---|---|---|
| Red Blood Cells | HSC → erythroblast → reticulocyte → mature erythrocyte | Bone marrow |
| White Blood Cells | – Myeloid line: HSC → myeloblast → myelocyte → granulocytes (basophils, eosinophils, neutrophils) – Myeloid line: HSC → monoblast → monocyte – Lymphoid line: HSC → lymphoblast → T-cells, B-cells, natural killer cells | Bone marrow and lymphoid tissues |
| Platelets | HSC → megakaryoblast → megakaryocyte → platelet fragments | Bone marrow |
The hematopoietic system needs a balance between self-renewal and differentiation. This balance keeps the blood supply healthy and steady.
Immune System Support
Hematopoietic stem cells help the immune system too. They make all the special immune cells that fight sickness. Self-renewal lets these cells keep the immune system strong for life. Differentiation helps them form T-cells, B-cells, and natural killer cells. These cells protect the body from germs.
Doctors use hematopoietic stem cells in bone marrow transplants. These transplants help rebuild weak immune systems. Patients get new immune cells that fight infections. The bone marrow is a safe place for hematopoietic stem cells. It protects them and helps control self-renewal and differentiation.
Note: Scientists study how hematopoietic stem cells react to signals and change into immune cells. This research helps make better treatments for diseases like cancer. Learning about self-renewal and differentiation helps doctors support the immune system in new ways.
Hematopoietic Stem Cell Transplantation
Treating Blood Disorders
Doctors use hematopoietic stem cell transplantation for many tough blood and immune disorders. This treatment swaps sick or damaged blood-forming cells for healthy ones. The new cells help the body make normal blood cells again. Hematopoietic stem cell therapy can cure or control diseases that do not get better with other treatments.
Some common blood and immune disorders treated with hematopoietic stem cell transplantation are:
- Thalassemia
- Anemias
- Sickle Cell Disease
- Severe Combined Immunodeficiency Disease (SCID)
- Wiskott-Aldrich Syndrome
- Krabbe Disease
- Hurler Syndrome
- Leukodystrophies
- Adrenoleukodystrophy (ALD)
- Severe Aplastic Anemia (SAA)
- Metachromatic Leukodystrophy (MLD)
Doctors also use hematopoietic stem cell therapy for some cancers, like leukemia and lymphoma. This therapy gives patients hope when other treatments do not work.
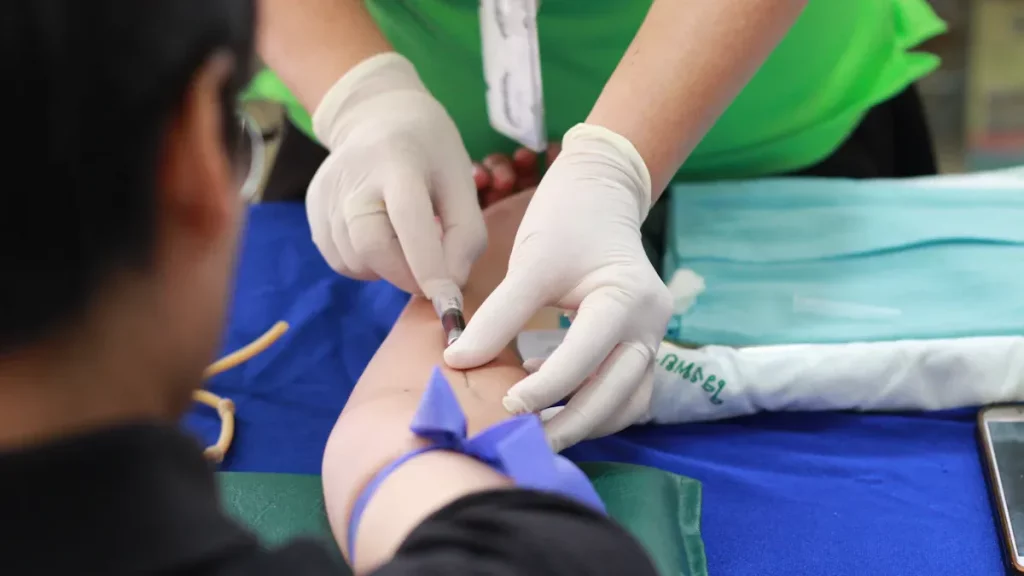
Transplantation Process
Hematopoietic stem cell transplantation has several important steps. Each step helps make the transplant work better.
- Donor Selection
Doctors look for a good donor. Donors can be family, volunteers, or cord blood units. The best donor is usually a close genetic match. This lowers the chance of problems. - Evaluation and Pre-transplant Testing
The medical team checks if the patient is ready for transplantation. They do tests to plan the best way to help. - Stem Cell Collection
Doctors collect hematopoietic stem cells from the donor. They use bone marrow, peripheral blood, or cord blood. Most adults get peripheral blood stem cells. Cord blood is often used for children. - Conditioning Treatment
The patient gets chemotherapy, radiation, or both. This kills sick cells and gets the body ready for new stem cells. - Stem Cell Infusion
The medical team puts the stem cells into the patient’s blood. This is a lot like a blood transfusion. - Neutropenic Phase
The patient’s immune system is very weak now. Doctors give antibiotics and other medicine to stop infections. - Engraftment and Recovery
The new hematopoietic stem cells go to the bone marrow. They start making new blood cells. Engraftment happens about 12 to 30 days after transplantation. Doctors check blood counts and watch for problems. - Post-transplant Care
The patient needs careful follow-up. Doctors look for issues like graft-versus-host disease, infections, and organ damage. Full immune recovery can take up to a year.
Tip: Patients must follow strict rules to avoid infection while healing. They may need to stay away from crowds, some foods, and pets for months.
The table below shows the main sources of hematopoietic stem cells and some differences:
| Source | Common Use | Advantages | Considerations |
|---|---|---|---|
| Bone Marrow | Children, some adults | Lower risk of GVHD | Slower engraftment |
| Peripheral Blood | Most adults | Faster engraftment | Higher risk of GVHD |
| Cord Blood | Children, no matched donor | Easy to collect, less strict matching | Lower cell dose, slower recovery |
Success Stories
Hematopoietic stem cell transplantation has saved many lives. Some people stay healthy for a long time or are even cured. For example, the “Berlin Patient” got a stem cell transplant from a donor with a special gene change. This led to long-term remission of HIV, showing how powerful hematopoietic stem cell therapy can be.
Children with leukemia have also been helped a lot. Recent studies show that kids with very high-risk acute lymphoblastic leukemia (ALL) have a 65% five-year survival rate after stem cell transplant. For acute myeloid leukemia (AML), the five-year survival rate is 74%. These numbers show how well hematopoietic stem cell transplantation works.
| Condition | 10-Year Overall Survival | 10-Year Disease-Free Survival | 10-Year Relapse Rate | 10-Year Non-Relapse Mortality |
|---|---|---|---|---|
| Acute Myelogenous Leukemia (AML) | 84% | 82% | 10% | 9% |
| Acute Lymphoblastic Leukemia (ALL) | 84% | 82% | 9% | 9% |
| Myelodysplastic Syndrome (MDS) | 80% | 78% | 10% | 12% |
| Lymphoma | 84% | 82% | 6% | 11% |
| Severe Aplastic Anemia (SAA) | 92% | N/A | N/A | N/A |
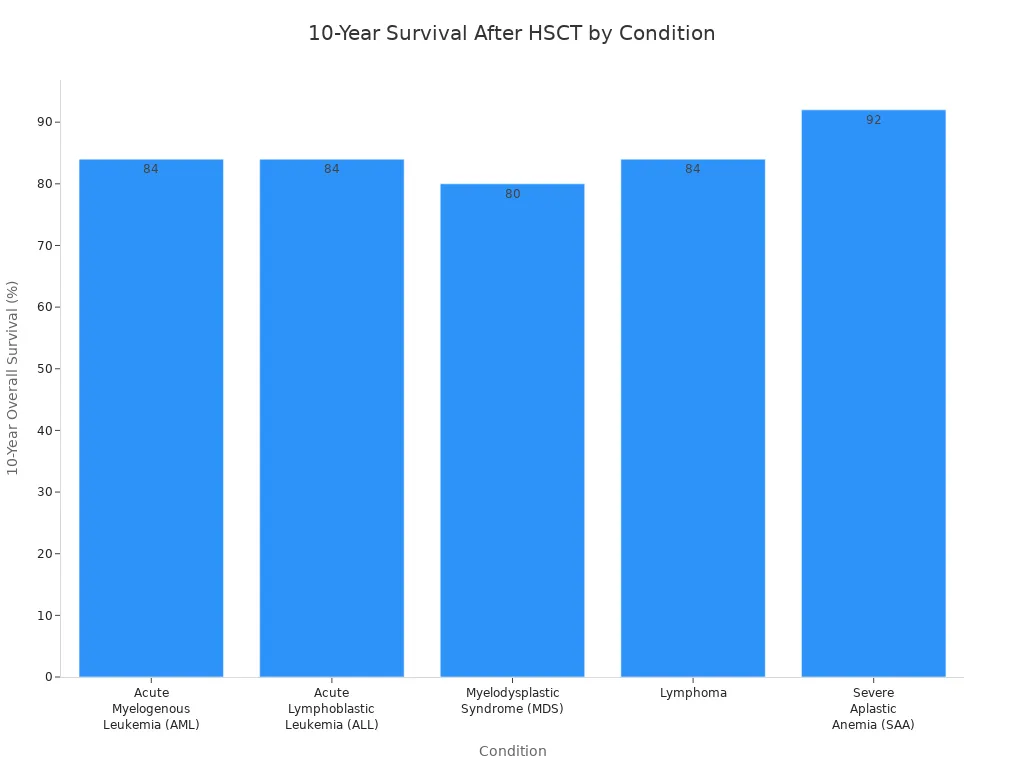
Doctors around the world do almost 90,000 hematopoietic stem cell transplants each year. The number keeps going up as more people get help from this life-saving therapy. Hematopoietic stem cell transplantation gives hope to people with diseases once thought untreatable. With more research and better care, more patients will keep surviving and living well after transplantation.
Future of Hematopoietic Stem Cells
Research Advances
Scientists are learning new things about hematopoietic stem cells. They found a process called c-Kit-associated trogocytosis. In this process, hematopoietic stem cells take membrane proteins from macrophages. This helps control if the cells stay in the bone marrow or move into the blood. If doctors can improve this, they might collect more hematopoietic stem cells for transplants. Right now, many medicines do not help release enough cells. This research could fix that problem.
Allogeneic transplantation has changed a lot since the 1950s. Doctors now pick better donors and use safer treatments before transplants. They also handle graft-versus-host disease better. These changes make hematopoietic transplantation safer and work better. Gene editing has also made hematopoietic therapies better. New tools like CRISPR-Cas9 and base editors can change DNA in hematopoietic stem cells. These tools help treat diseases like sickle cell disease and thalassemia. Clinical trials now use these tools to fix single gene problems. Researchers are working on safer and better ways to use gene editing in hematopoietic therapies.
Expanding Treatment Options
Hematopoietic stem cell therapies now help more diseases than before. Doctors use these therapies for blood disorders, immune problems, and some cancers. The list of conditions includes:
- Primary immune deficiencies like ADA-deficient Severe Combined Immunodeficiency (SCID), X-linked SCID, and Wiskott-Aldrich Syndrome
- Hemoglobinopathies like sickle cell disease and beta-thalassemia
- Storage and metabolic disorders like Gaucher Disease and Mucopolysaccharidoses
- Congenital cytopenias and stem cell defects, such as Fanconi Anemia and Schwachman-Diamond Syndrome
- Engineered T cell therapies for some cancers
Many hematopoietic therapies are in early clinical trials or already approved. Strimvelis is one therapy for ADA-deficient SCID. The market for hematopoietic stem cell therapy is growing fast. Experts think it will almost double in the next ten years. More research, better donor matching, and new gene editing tools help this growth.
There are still problems with hematopoietic therapies. Doctors have trouble finding enough matched donors, growing cells outside the body, and lowering costs. The table below shows some of the biggest problems for the future:
| Challenge Area | Details |
|---|---|
| Donor Availability | Not enough HLA-matched donors, especially for some groups |
| Cell Expansion | Hard to grow enough hematopoietic stem cells for treatment |
| Transplant Risks | Graft rejection, graft-versus-host disease, and immune complications |
| Gene Editing | Need for safer, more efficient editing and long-term safety data |
| Accessibility | High costs limit who can get these treatments |
Note: New research and technology will help solve these problems. The future of hematopoietic stem cell therapy looks good as scientists find more ways to help patients and make treatments better.
Getting a transplantation can give people a fresh start. Life often gets better after transplantation. But healing takes time and help from others. Many people do not know much about transplantation. That is why learning and teaching others is important. People can help by signing up as donors. They can also join events or tell others about transplantation. New research and better care keep making transplantation safer. More people are living well after transplantation. The future looks good for transplantation.
- Ways to support transplantation:
- Join a donor registry
- Advocate for awareness
- Support patient programs
FAQ
What is a hematopoietic stem cell transplant?
A hematopoietic stem cell transplant swaps sick blood-forming cells for healthy ones. Doctors use this for diseases like leukemia and lymphoma. Some immune disorders are also treated this way. The new cells help the body make normal blood cells.
Who can donate hematopoietic stem cells?
Doctors need donors who match the patient’s tissue type. Family members can be donors. Unrelated volunteers or cord blood units can also help. Many people join donor registries to help others.
Is the donation process painful?
Most donors feel a little sore or tired. Doctors use medicine to collect stem cells from blood or bone marrow. Most people feel better soon after donating.
How long does recovery take after a transplant?
Recovery time is different for everyone. Most patients stay in the hospital for weeks. It can take months for the immune system to get strong again. Doctors watch patients closely during this time.
Can hematopoietic stem cell transplants cure diseases?
Yes, transplants can cure some blood cancers and genetic problems. Success depends on the disease and the patient’s health. It also depends on how well the donor matches. Many people live healthy lives after a good transplant.