When I think about stem cell therapy, I am amazed by science. Stem cells, harvested from sources like bone marrow, blood, and umbilical cords, are collected using special methods to ensure precision. For example, new iPSC technology is revolutionizing cell therapy. After years of study, experts now rely on advanced machines and strict protocols. This approach helps harvest more cells for treating diseases safely and accurately.
Sources of Stem Cells
Bone Marrow
Bone marrow is a well-known source of stem cells. It is the soft tissue inside large bones like hips and thighs. This tissue has many blood stem cells, which help treat diseases. These cells can grow into new blood cells, making them very useful for treatments like transplants.
Studies show bone marrow works better for younger patients. For example, kids under 20 have a 90% survival rate with it. In comparison, using peripheral blood stem cells gives a 76% survival rate. Even older patients live 10-14% longer with bone marrow transplants. This makes it a good choice for certain age groups.
Still, bone marrow harvesting is not the most common method. A table shows that bone marrow is used in 54% of cases. Peripheral blood is used in 41%, and cord blood in only 5%.
| Source of Stem Cells | Percentage (%) |
|---|---|
| Bone Marrow | 54% |
| Peripheral Blood Stem Cells | 41% |
| Cord Blood | 5% |
Peripheral Blood
Peripheral blood is another key source of stem cells. These stem cells float in the bloodstream, unlike those in bone marrow. To collect them, doctors use a process called apheresis. Blood is taken, stem cells are removed, and the rest of the blood goes back to the donor. This method is easier and less painful than bone marrow collection.
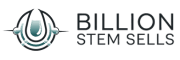
Peripheral blood is the top choice for autologous transplants. It is used in 100% of these cases. It also works well, as shown in the chart below:
However, peripheral blood is not always the best option. For younger patients, bone marrow still gives better survival rates.
Umbilical Cord Blood
Umbilical cord blood is an amazing source of stem cells. After a baby is born, the leftover blood in the cord and placenta is collected. This blood has special stem cells that adapt easily and rarely cause immune problems. It is great for treating genetic diseases and cancers.
Cord blood is not used as often as other sources. But it has some unique benefits. It is easy to collect and can be stored in banks for later use. This makes it helpful for families and scientists.
Adipose Tissue and Other Sources
Body fat, called adipose tissue, is a surprising stem cell source. This fat, often removed during liposuction, can help in medicine. Adipose-derived stem cells (ADSCs) are easy to collect and plentiful. These cells can turn into bone, cartilage, or fat cells. Their flexibility makes them useful for healing and repair.
Getting stem cells from fat is simple and less painful. Unlike bone marrow, it causes little discomfort for donors. The process is quick and uses local anesthesia. This makes it a good choice for patients and scientists.
Research shows fat tissue stem cells work well. Cells from different fat areas act in similar ways. They share traits like appearance, survival, and ability to change. The table below shows these findings:
| Fat Area | Appearance | Survival | Ability to Change |
|---|---|---|---|
| Area 1 | Similar | Same | Turns into fat, bone, or cartilage |
| Area 2 | Similar | Same | Turns into fat, bone, or cartilage |
| Area 3 | Similar | Same | Turns into fat, bone, or cartilage |
| Area 4 | Similar | Same | Turns into fat, bone, or cartilage |
| Area 5 | Similar | Same | Turns into fat, bone, or cartilage |
Other stem cell sources include dental pulp, amniotic fluid, and hair. These options give more ways to study and use stem cells. As science grows, we may find even better uses for these cells. For now, fat tissue is one of the easiest and most promising sources.
Procedures for Harvesting Stem Cells
Bone Marrow Aspiration
Bone marrow aspiration is a traditional way to collect stem cells. Doctors use a hollow needle to take marrow from large bones, like the hip. This is done under anesthesia so the donor feels little pain. The process is careful to get as many stem cells as possible.
Different methods can change how well this works. For example, the reorientation method collects more CD34+ cells than the usual way. The table below shows the differences:
| Metric | Conventional Technique | Reorientation Technique | p-value |
|---|---|---|---|
| Leucocytes per nl | 5 ± 2 | 12 ± 4 | < .001 |
| CD 34+ cells per μl | 40 ± 40 | 140 ± 98 | .003 |
This data shows better techniques can improve stem cell collection. Bone marrow aspiration is still important, especially for younger patients, because it works well for them.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is less painful than bone marrow aspiration. Medications like G-CSF move stem cells from the marrow into the blood. Doctors then use apheresis to separate the stem cells from the blood. The rest of the blood goes back to the donor.
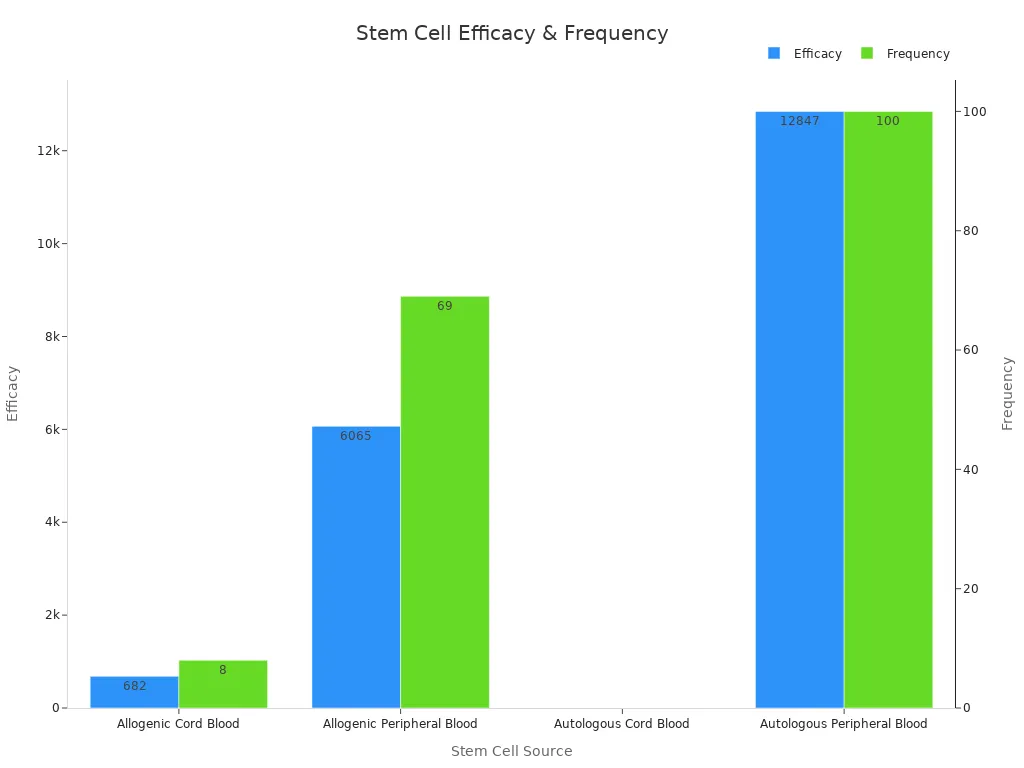
This method is often used for autologous transplants. Studies show it works well. For example, combining cyclophosphamide with G-CSF collects more CD34+ cells faster than using G-CSF alone. The chart below shows these results:
Donor factors like age, gender, and weight can affect success. Male donors and heavier donors often have better results. This method is efficient and helpful for many patients.
Umbilical Cord Blood Collection
Umbilical cord blood collection is simple and exciting. After a baby is born, blood from the cord and placenta is collected. This blood has special stem cells that adapt easily and rarely cause immune problems. The process is easy and painless, making it a good choice for families.
The total nucleated cell count (TNC) in cord blood is important. TNC counts between 2 × 10^8 and 4 × 10^8 per kilogram are best for success. Lower counts can slow recovery and raise infection risks. Factors like the baby’s weight, gender, and delivery method can affect the amount and quality of cord blood.
Cord blood collection is valuable for therapy and research. It can be stored for future use, helping families and scientists in many ways.
Mobilization Techniques and Equipment
When I first heard about mobilization techniques, I was amazed. Science helps move stem cells from bone marrow to the bloodstream. This makes collecting them much easier. It’s an important step, especially for using peripheral blood as a source.
Techniques for Moving Stem Cells
Doctors use different ways to move stem cells. Each method works best depending on the patient and transplant type. Here are the most common methods:
- Growth Factor Injections
Growth factors, like G-CSF, are special proteins. They help the bone marrow make more stem cells. These proteins push the cells into the bloodstream. This method is safe and works well for most people. Healthy donors often use this option. - Chemotherapy-Induced Mobilization
Chemotherapy can also help move stem cells. Some drugs make the bone marrow release these cells into the blood. Doctors often add growth factor injections to collect even more cells. - Plerixafor (CXCR4 Inhibitor)
Plerixafor is a medicine that helps stem cells leave the bone marrow. It blocks a receptor, making the cells move into the bloodstream. This is helpful for people who don’t respond well to growth factors alone. - Combination Approaches
Sometimes, doctors mix methods for better results. For example, using G-CSF with plerixafor collects more stem cells. This is useful for patients with harder-to-move cells.
Tools Used for Mobilization and Collection
Special tools make stem cell collection safe and effective. Here are some commonly used ones:
- Apheresis Machines
These machines separate stem cells from blood. Blood is taken, processed, and returned to the donor. It’s amazing how precisely these machines work. - Injection Devices
These devices give growth factors and other medicines. They ensure the right dose is given for success. - Monitoring Equipment
Doctors use monitors to check the donor’s health and stem cell levels. This keeps the process safe and effective.
Tip: Drinking water and resting can help the process. Donors should stay hydrated and follow their doctor’s advice.
Factors That Affect Success
Many things affect how well stem cells move. These include age, health, and past treatments. Younger donors usually respond better to growth factors. Patients with heavy chemotherapy may need extra help, like plerixafor.
Mobilization techniques and tools have improved a lot. They make collecting stem cells easier and safer. It’s inspiring to see how these advancements help both patients and donors.
Patient Considerations During Harvesting Stem Cells
Anesthesia and Pain Management
Patient comfort is very important during stem cell harvesting. For bone marrow aspiration, doctors use general or local anesthesia. This helps reduce pain during the procedure. Peripheral blood collection usually doesn’t need anesthesia because it is less invasive.
New pain management methods have made these procedures safer. A study showed less medication was needed with updated protocols. The table below shows how medication use dropped:
| Parameter | Before Implementation (Median, IQR; min-max) | After Implementation (Median, IQR; min-max) | P-value |
|---|---|---|---|
| Intraoperative MME | 20.0 (12.5; 0–37.5) | 0.0 (0.0; 0–6.25) | <0.001 |
| PACU MME | 5.0 (8.0; 0–24) | 0.0 (0.0; 0–16) | 0.073 |
| Total MME | 20.5 (22.3; 0–57) | 0.0 (0.0; 0–16) | <0.001 |
These results show how modern techniques make patients more comfortable.
Recovery and Aftercare
Recovery depends on the harvesting method used. Bone marrow donors may feel sore for a few days. Peripheral blood donors might feel a little tired. Rest and drinking water are very important for recovery.
Blood cell recovery happens quickly after transplantation. Neutrophil levels (≥0.5 × 10^9/L) return by day 14. Platelet levels (≥20 × 10^9/L) recover in 10–11 days. Higher platelet levels (≥50 × 10^9/L) are reached by day 13–14. These timelines show that proper care helps patients recover fast.
Tip: Eat foods with iron and vitamins to heal faster. Always follow your doctor’s advice after the procedure.
Risks and Side Effects
All medical procedures have risks, and stem cell harvesting is no different. Bone marrow aspiration may cause short-term pain or bruising. Peripheral blood collection can lead to mild side effects like headaches or tingling from calcium loss. Serious problems, like infection or bleeding, are rare.
Mobilization techniques, like using plerixafor, have made the process safer. For example:
- Plerixafor raises CD34+ cell counts by 312%.
- It lowers the chance of mobilization failures.
- However, it may delay platelet recovery (p = 0.029).
These improvements make stem cell harvesting safer. With careful monitoring and advanced methods, risks are reduced, and benefits are increased for patients.
Applications of Stem Cells Harvested
Stem Cell Therapy for Blood Disorders
Stem cell therapy has changed how blood disorders are treated. Diseases like leukemia, lymphoma, and sickle cell anemia now have better outcomes. Stem cell transplants replace unhealthy blood cells with healthy ones. This helps the body make normal blood cells again.
There are two main types of transplants. In an autologous transplant, patients use their own stem cells. These cells are collected and stored before treatment, lowering the chance of rejection. In an allogenic transplant, stem cells come from a donor. This method works better for some conditions.
The results of these therapies are well-studied. Groups like CIBMTR share reports on survival rates and trends. These reports guide doctors and researchers in making decisions. Below is a summary of key resources:
| Resource | Description |
|---|---|
| CIBMTR Summary Slides & Reports | Shares data on outcomes and trends for better decisions. |
| US Summary Slides – Trends and Survival Data | Shows yearly charts on therapy uses and results. |
| US Patient Survival Report | Gives survival estimates after transplants at different times. |
| US Transplant Data by Disease Report | Lists transplant numbers for diseases with demographic details. |
These resources show how stem cell therapy saves lives. This field is growing and bringing hope to more patients.
Regenerative Medicine and Tissue Repair
Stem cells are also helping repair damaged tissues. They offer new treatments for injuries and diseases once thought untreatable. For example, they are used for knee osteoarthritis, tendon injuries, and degenerative disc disease.
The success rates of these treatments are high. For knee osteoarthritis, success rates range from 70-85%. Tendon injuries like tennis elbow see 75-80% success. Below is a table of success rates for various conditions:
| Condition | Success Rate (%) |
|---|---|
| Knee Osteoarthritis | 70 – 85 |
| Tendon Injuries (e.g., Tennis Elbow) | 75 – 80 |
| Degenerative Disc Disease | 60 – 75 |
| Chronic Low Back Pain | 50 – 65 |
| Stroke Recovery | 40 – 60 |
| Autoimmune Conditions (e.g., Rheumatoid Arthritis) | 60 – 75 |
| Overall Average | ~78 |
These therapies improve physical function and quality of life. Stem cells’ ability to heal tissues makes them a game-changer. Regenerative medicine is one of the most exciting areas in healthcare today.
Contribution to Clinical Trials and Research
Stem cells are vital for advancing medical research. Clinical trials using these cells often show positive results. About 67.3% of trials report success, proving the promise of stem cell therapy.
For joint repair and autoimmune diseases, success rates reach 80%. These results give hope for future treatments. Researchers are finding new ways to use stem cells. They aim to create personalized therapies and test treatments for tough diseases.
Note: Clinical trials help improve treatments and lead to discoveries. Patients in these trials help develop therapies that could help many others.
Data from these studies is very important. It improves techniques, boosts safety, and expands treatment options. Stem cells’ role in research is transforming medicine. They bring hope for conditions without good treatments today.
Getting stem cells is very important for modern medicine. Methods like bone marrow, blood, and cord blood collection are safe and effective. These techniques have changed how we treat blood diseases, fix tissues, and more.
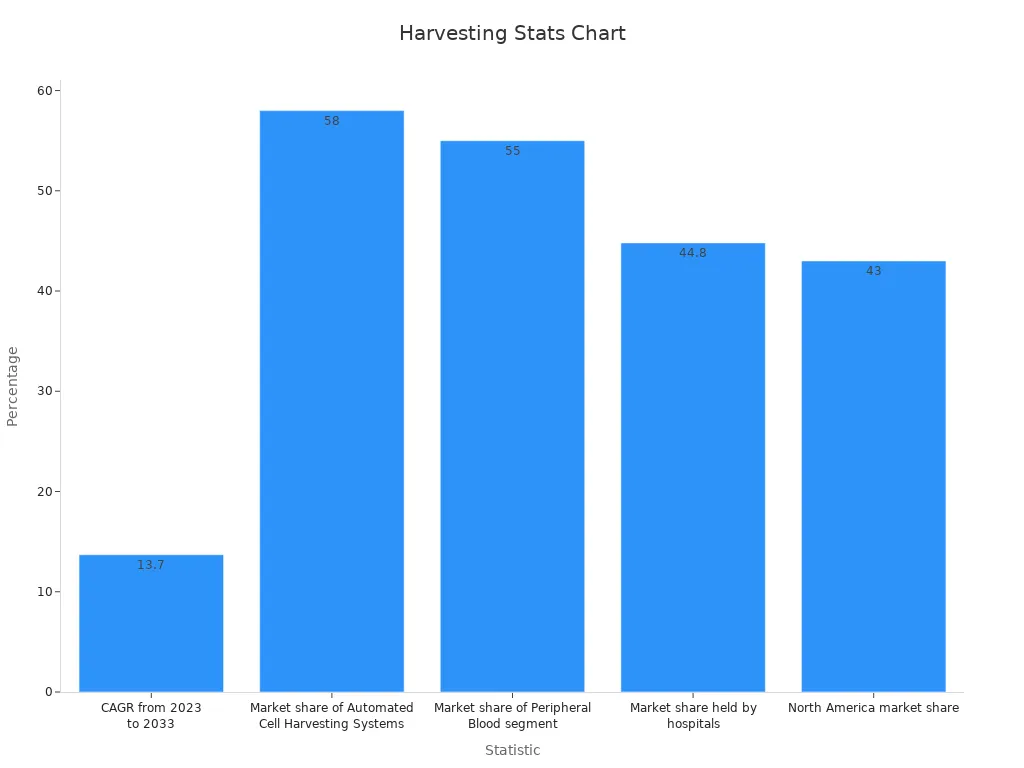
Better ways to collect stem cells are boosting the market. By 2033, the global stem cell market could reach $13 billion. It is growing fast, with a yearly growth rate of 13.7%. Machines for automatic cell collection lead with 58% of the market. Stem cells from blood make up 55%, and hospitals hold 44.8%. North America is ahead with 43% of the market, worth $1.5 billion in 2023.
| Statistic Description | Value |
|---|---|
| Projected market value by 2033 | $13 billion |
| Yearly growth rate (CAGR) from 2023 to 2033 | 13.7% |
| Market share of automated cell systems | 58% |
| Market share of blood stem cells | 55% |
| Market share held by hospitals | 44.8% |
| North America market share | 43% |
| North America market value in 2023 | $1.5 billion |
Stem cell therapy has changed healthcare, giving hope for hard-to-treat illnesses. With new ideas and tools, the future looks very promising.