Stem cells originate as key components in modern medicine that repair the body. These special cells come from embryos, adult tissues, or labs. They can change into different cell types to fix damage. For instance, stem cell transplants help many patients survive diseases. Hodgkin lymphoma patients have a 92% survival rate after three years. Multiple myeloma patients have a 79% survival rate. These numbers show how powerful stem cells are in medicine. Understanding where stem cells originate helps us see their importance in science and health.
- Key Takeaways
- Types of Stem Cells
- Sources and Ways to Collect Stem Cells
- Applications in Regenerative Medicine
- Ethical and Practical Considerations
- FAQ
Key Takeaways
- Stem cells help the body heal by becoming different cell types.
- There are embryonic, adult, iPSCs, and perinatal stem cells.
- Each type has special features and helps treat diseases.
- Stem cell treatments work well, with 92% survival for Hodgkin lymphoma.
- iPSCs use adult cells, making them safer and more ethical.
- Stem cell treatments are expensive and not well-known to many people.
- More education and teamwork can improve access to these treatments.
Types of Stem Cells
Learning about stem cells helps us understand their role in medicine. Each type has special traits, origins, and uses.
Embryonic Stem Cells
What they are and what they can do
Embryonic stem cells come from very early embryos. These cells can turn into almost any cell in the body. This makes them very useful for fixing damaged tissues. For example, they may help treat diseases that other treatments cannot cure. Their ability to grow and change gives hope for healing organs and tissues.
Where embryonic stem cells come from
These cells are taken from embryos about five days old. These embryos are often left over from IVF treatments. Scientists carefully remove the inner part of the embryo, which holds these special cells. This shows how stem cells can change healthcare.
- Important facts about embryonic stem cells:
- Taken from early embryos.
- Can become many cell types.
- May help treat hard-to-cure diseases.
Adult Stem Cells
What they do and why they matter
Adult stem cells help repair and maintain tissues. Unlike embryonic stem cells, they can only turn into certain cell types. For example, bone marrow stem cells make blood cells. Other adult stem cells help fix bones, cartilage, or fat. These cells are important for keeping our bodies healthy.
Where adult stem cells are found
Adult stem cells come from places like bone marrow, fat, and the brain. Bone marrow is a common source for these cells. Fat tissue from liposuction is also used to get stem cells. These cells are becoming more popular in medical treatments. The table below shows key findings about adult stem cells:
| Evidence Description | Source | Year |
|---|---|---|
| Adult stem cells help repair tissues and keep them healthy. | Emmrich et al. | 2024 |
| Mesenchymal stem cells may help treat brain diseases. | Guy and Offen | 2020 |
| Stem cell treatments may fight aging and improve health. | Rudnitsky et al. | 2024 |
Induced Pluripotent Stem Cells (iPSCs)
What they are and how they are made
Induced pluripotent stem cells are adult cells changed in labs to act like embryonic stem cells. Scientists add certain genes to reset the cells. iPSCs can turn into many cell types, just like embryonic stem cells. This method avoids ethical issues linked to using embryos.
How they help in medicine
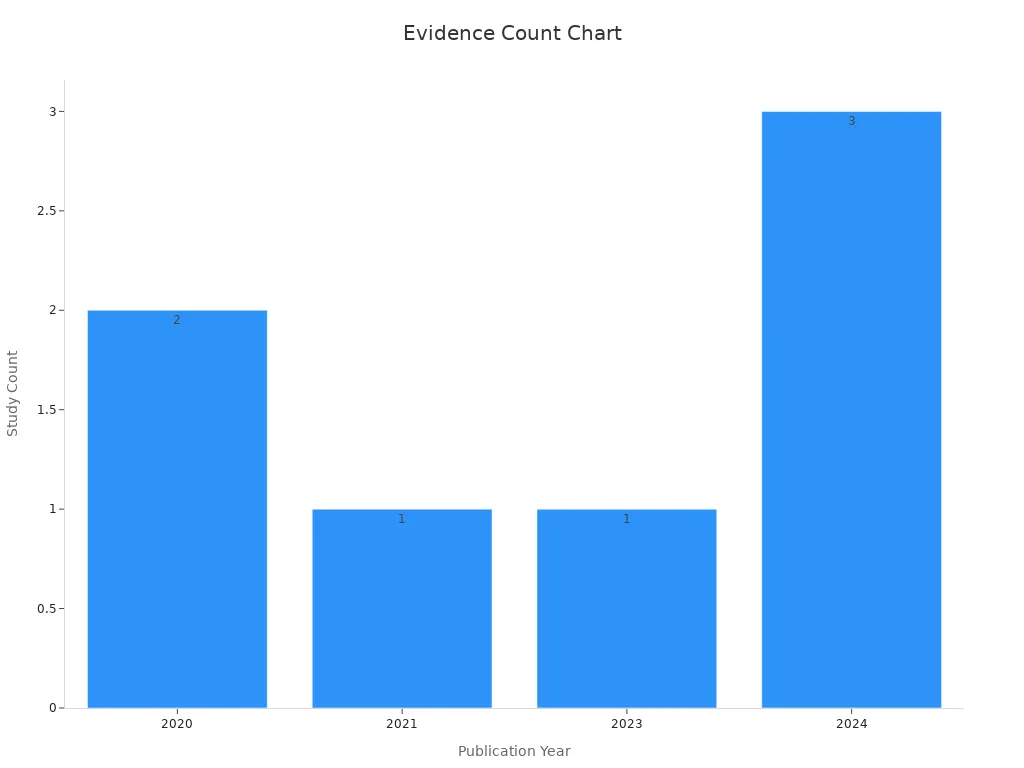
iPSCs are very useful in medicine. They allow doctors to use a patient’s own cells, lowering the chance of rejection. New lab methods have made creating iPSCs much easier. For example, better lab conditions have made the process 100 times more efficient. The chart below shows how research on iPSCs is growing:
Perinatal Stem Cells
Traits and uses
Perinatal stem cells come from tissues around a baby at birth. These include the umbilical cord and placenta. They are special because they act like embryonic stem cells but with fewer ethical issues. These cells can turn into many types, like bone, nerve, or cartilage cells. This makes them helpful for treating injuries and diseases.
One amazing feature is their ability to fix damaged tissues. For example, scientists study them to repair spinal cord injuries and treat blood problems. They may also reduce swelling, which could help with autoimmune diseases.
Note: Perinatal stem cells are collected without harming the baby or donor. This makes them an ethical and easy-to-get option for research and treatments.
Where they come from: Umbilical cord and placenta
The umbilical cord and placenta are full of perinatal stem cells. After birth, these tissues are often thrown away. But they have great medical value.
- Umbilical cord blood: This blood has hematopoietic stem cells that make new blood cells. Doctors use them to treat illnesses like leukemia and anemia.
- Placenta: The placenta has mesenchymal stem cells that can become bone, cartilage, or muscle cells. These are being studied for healing damaged tissues.
Families can store umbilical cord blood in private or public banks. This ensures these useful cells are saved for future needs. Collecting placental tissue is also becoming more common in research.
Perinatal stem cells are both flexible and easy to access. Their potential to change medicine grows as studies continue.
Sources and Ways to Collect Stem Cells
Where Embryonic Stem Cells Come From
Using blastocysts from IVF
Embryonic stem cells come from blastocysts, which form 5–6 days after fertilization. These blastocysts are often from embryos made during IVF treatments. When families no longer need these embryos, they can donate them for research. This gives scientists a way to get stem cells without creating new embryos just for studies.
Inside the blastocyst is a group of cells called the inner cell mass. These cells can turn into almost any type of cell in the body. They are very important for studying diseases, testing medicines, and finding new treatments. For example, scientists use blastocysts left after genetic testing to study genetic problems. This method helps science grow without wasting embryos.
How Adult Stem Cells Are Collected
Getting stem cells from bone marrow
Bone marrow has many adult stem cells, especially ones that make blood cells. Doctors take marrow from the pelvic bone using a needle. This process, called bone marrow aspiration, is done under anesthesia to avoid pain.
The success of treatments using these cells depends on their quality. Using a patient’s own marrow lowers the chance of rejection. But there are some risks, like infection or problems with anesthesia. Even with these risks, bone marrow collection is key for treating blood diseases.
Collecting stem cells from fat tissue
Fat tissue, also called adipose tissue, is another source of adult stem cells. These cells are taken out using liposuction, a simple and less painful procedure. Fat-derived stem cells can turn into bone, cartilage, or muscle cells. This makes them useful for fixing injuries and damaged tissues.
Liposuction is safer and less invasive than bone marrow collection. It also provides a large number of stem cells. Because of this, it is becoming a popular way to collect stem cells for medical use.
Collecting Perinatal Stem Cells
Saving umbilical cord blood
Umbilical cord blood has many stem cells that make blood cells. After a baby is born, doctors collect the leftover blood from the cord. This is stored in special banks. The process is safe for both the mom and baby. Families can keep the cord blood in private banks or donate it to public ones for others to use.
Cord blood stem cells are used to treat diseases like leukemia and anemia. They work well in transplants, especially for blood cancers. Since they are collected ethically, many researchers prefer using them.
Gathering stem cells from the placenta
The placenta, usually thrown away after birth, has many stem cells. These cells can grow into bone, cartilage, or muscle tissues. Collecting placental tissue does not harm the mom or baby, making it an easy and ethical option.
Scientists are studying placental stem cells for treating joint problems and autoimmune diseases. These cells are easy to collect and very flexible, making them a great resource for future treatments.
Induced Pluripotent Stem Cell Creation
Changing adult cells in the lab
Making induced pluripotent stem cells means changing adult cells to act like embryonic stem cells. Scientists do this by adding special genes to the adult cells. These genes help the cells reset and turn into different types of cells. This method avoids ethical problems linked to embryonic stem cells.
The process uses specific tools, like proteins or chemicals, to turn on the needed genes. For instance, scientists often use fibroblasts, which are cells found in connective tissue. By adding these tools, fibroblasts change into pluripotent cells. These new cells can become heart, nerve, or muscle cells.
Over time, scientists have made this process faster and more reliable. Early research, like Takahashi et al. (2006), showed it was possible to reprogram mouse cells. Later, Takahashi et al. (2007) and Yu et al. (2007) proved it worked with human cells too. These discoveries helped create today’s advanced methods.
Here’s a quick look at important studies about reprogramming:
| Study | Findings |
|---|---|
| Takahashi et al. (2006) | Mouse cells turned into pluripotent stem cells using defined factors. |
| Takahashi et al. (2007) | Human fibroblasts reprogrammed into pluripotent stem cells. |
| Yu et al. (2007) | Human somatic cells made into induced pluripotent stem cell lines. |
| Shi et al. (2008) | Combined chemical and genetic methods for making pluripotent cells. |
| Li et al. (2009) | Rat and human cells reprogrammed using genes and chemical inhibitors. |
| Mali et al. (2008) | Faster and better ways to make pluripotent cells from fibroblasts. |
These studies show how far reprogramming has come. They also highlight the use of induced pluripotent stem cells in medicine. With this technology, doctors can create cells from a patient’s body. This lowers the chance of the body rejecting treatments.
Note: Changing adult cells is a detailed process but offers great promise. It mixes science with ethics, opening doors to amazing medical progress.
Applications in Regenerative Medicine
Tissue Regeneration
Fixing damaged tissues and organs
Stem cells are key to fixing damaged tissues and organs. They can change into specific cells to treat injuries and diseases. For example, mesenchymal stem cells (MSCs) help rebuild cartilage and bone. This is helpful for people with joint injuries or osteoarthritis.
New progress in regenerative medicine shows how powerful stem cells are. Stem cell transplants already treat blood diseases and cancers like Hodgkin lymphoma. The table below shows success rates for stem cell therapies:
| Condition | Success Rate (%) | Notes |
|---|---|---|
| Multiple Myeloma | 79 | Three-year survival rate with autologous stem cell transplants. |
| Hodgkin Lymphoma | 92 | Survival rate three years post-transplant for patients post-chemotherapy. |
| Non-Hodgkin Lymphoma | 72 | Survival rate three years post-transplant for recurrent disease. |
| Osteoarthritis | N/A | MSC therapy shows promise but specific rates are under investigation. |
| Multiple Sclerosis | N/A | Positive results in clinical trials, but specific success rates vary. |
| Graft Versus Host Disease (GvHD) | N/A | Indicated positive outcomes in clinical trials. |
These numbers show how stem cell treatments are improving medicine. They open doors to new ways of healing.
Disease Treatment
Helping with diseases like leukemia, Parkinson’s, and diabetes
Stem cell therapy is changing how we treat hard-to-cure diseases. For leukemia, stem cells replace sick blood cells with healthy ones. This slows the disease and helps patients live longer. In Parkinson’s disease, scientists study how stem cells can fix damaged brain cells. This might reverse symptoms. For diabetes, stem cells could help make insulin-producing cells again. This gives hope to people who need daily insulin shots.
Stem cells also help with nerve problems, like spinal cord injuries. Mesenchymal stem cells can replace damaged cells and reduce swelling. These successes show how stem cells can solve many health problems.
Drug Testing and Development
Testing new medicines with stem cells
Stem cells, especially iPSCs, are changing how we test medicines. Unlike old methods, iPSCs let scientists study diseases and test drugs better. Scientists can turn iPSCs into specific cells to check how drugs work.
This helps create treatments that fit each person’s needs. For example:
- iPSCs show how drugs affect certain cells, making tests more accurate.
- They help study rare diseases that are often ignored in regular tests.
- Using iPSCs from patients helps find side effects early, making trials safer.
Stem cell drug testing speeds up finding safer and better medicines. It also improves how treatments are made for everyone.
Advancing Scientific Research
Learning about human growth and diseases
Stem cells have changed how we study human growth and illnesses. Their ability to become different cell types is amazing. This helps scientists learn how cells grow, change, and work together. By watching these steps, we understand how tissues and organs are made. This knowledge shows us the causes of genetic problems and developmental disorders.
Embryonic stem cells (ESCs) are very useful for this research. They can turn into any cell type, helping us study early human growth. Scientists use ESCs to see how cells change and form complex structures. Induced pluripotent stem cells (iPSCs) are also important. These are adult cells reprogrammed to act like ESCs. They carry a person’s genetic details, making them great for studying diseases and testing treatments for specific genes.
Adult stem cells are more limited but still helpful for studying tissues. For example, mesenchymal stem cells (MSCs) from bone marrow or fat can become bone, cartilage, or muscle cells. Scientists use MSCs to learn how tissues heal after injuries.
Organoids are tiny 3D models of organs made from stem cells. They act like real organs, letting scientists study diseases in labs. For example, organoids help us learn how cancer starts or how infections spread in tissues.
- Key ways stem cells help research:
- ESCs show early growth stages.
- iPSCs help study personal diseases.
- Adult stem cells explain tissue healing.
- MSCs aid regenerative medicine research.
- Organoids copy organ functions for disease studies.
Stem cells connect basic science to medical uses. They help us understand human biology and create new treatments.
Ethical and Practical Considerations
Ethical Concerns
Issues with using embryonic stem cells
Using embryonic stem cells causes many ethical arguments. These cells come from early embryos, which some people find wrong. They believe using embryos for science disrespects potential life. Others think saving lives makes it acceptable.
Clear rules are needed to address these concerns. Some countries, like the U.S., limit funding for this research. Others, like the U.K. and Sweden, allow more freedom for scientists. Balancing ethics and progress is still a big challenge.
Safety and Risks
Risks of tumors and immune system rejection
Stem cell treatments are promising but have risks too. Tumors can form after treatments. For example:
- A man got a tumor 12 years after a stem cell therapy.
- This shows untested treatments can cause serious problems.
- Tumors may take years to appear, so long-term checks are needed.
Another risk is immune rejection. If stem cells come from donors, the body might attack them. This can make treatments less effective. Careful testing and rules are needed to keep patients safe.
Regulations and Guidelines
Rules for stem cell research
Stem cell research laws differ around the world. In the U.S., strict rules limit funding for embryonic stem cell studies. This slows down research. But countries like the U.K. and Sweden have more flexible laws. They allow scientists to explore new treatments while following ethical rules.
Countries with fewer restrictions often make faster discoveries. Even so, they still follow strict guidelines to ensure safety and ethics. Clear laws help protect patients and support scientific progress.
Accessibility and Cost
Problems with making stem cell treatments available to everyone
Stem cell treatments are very promising but hard to access. The cost of these therapies is often too high for most people. For example, one session can cost tens of thousands of dollars. This is because the process is complex and needs special labs. A lot of money also goes into research and development.
Access to stem cell treatments depends on where you live. North America is ahead due to advanced healthcare and research funding. Europe is close behind, helped by government support and good rules. Other areas face big challenges. In Latin America and Africa, lack of money and unclear rules make access hard. Countries like Brazil and Argentina are improving but still struggle with costs and facilities. In Asia, countries like China and Japan are investing more in healthcare and research.
Note: Access isn’t just about money or location. Many people don’t know about stem cell treatments or how they can help. This shows the need for better education and awareness programs.
To make these treatments easier to get, we need teamwork. Governments and private groups should work together to lower costs. They also need to improve healthcare systems and set clear rules. This way, more people can benefit from these life-changing therapies, no matter where they live or how much money they have.
Stem cells come from embryos, adult tissues, or lab methods. They can turn into different cell types, helping in medicine.
- Stem cells help heal injuries and treat long-term diseases.
- They lower swelling and improve how the immune system works.
- Survival rates show their success:
- 92% for Hodgkin lymphoma patients after transplants.
- 79% for multiple myeloma patients using their own stem cells.
The stem cell therapy market may grow beyond $2.6 billion by 2033. Even with challenges, progress shows their amazing potential in healthcare.