Pluripotent stem cells can turn into any cell in the body. These cells show up early when an embryo is forming. They are not yet specialized. This lets them make all types of human cells, like neurons, blood cells, and muscle cells. Scientists think pluripotent stem cells are important. They can make copies of themselves forever. This gives many chances for research and medicine. Induced pluripotent stem cells were a big discovery. They help with disease modeling, drug testing, and new treatments. This shows how much they can help people.
Pluripotent Stem Cells
Definition
Pluripotent stem cells are found early in an embryo. They come from the inner cell mass of a blastocyst, which is a very young embryo. These cells have not changed into any special type yet. They can become almost any cell in the body, like nerve, muscle, or liver cells. The NIH says pluripotent stem cells can make all the cell types in an adult body. This includes cells from three main germ layers: ectoderm, mesoderm, and endoderm. These layers help form all tissues and organs. Pluripotent stem cells can also make germ cells, which are needed for reproduction. Scientists call them “true stem cells” because they can do so much.
Unique Features
Pluripotent stem cells have special traits that make them different from other cells. First, they can self-renew. This means they can copy themselves for a long time without changing. Second, they can go through differentiation. This lets them turn into any cell from the three germ layers. These abilities make them very useful for research and medicine.
Their special traits come from certain molecules inside the cells. These include transcription factors like Oct4, Sox2, and Nanog. These molecules help the cells stay as stem cells and control when they change into other types. Scientists use tests to see if a cell is really pluripotent. They look for special markers on the cell surface. They also test if the cells can make all three germ layers in the lab. Sometimes, they check if the cells can form teratomas, which are growths with many tissue types, when put in mice. These tests help prove the special features of pluripotent stem cells.
Key Characteristics
Self-Renewal
Pluripotent stem cells can make copies of themselves. They divide many times and stay the same. These cells keep their special features after dividing. Many things help them keep this ability. Signals from outside the cell, transcription factors, and cell-cycle regulators are important. MicroRNAs and genes that keep chromosomes safe also help. DNA methylation controls which genes are on or off. The right balance of signals is needed for survival and growth. Myc is a key transcription factor. Histone H3.3 is an epigenetic regulator. Both help control gene activity. Myc helps keep stem cells working and helps make induced pluripotent stem cells. But if Myc is not controlled, it can cause tumors. Scientists keep studying these things to make stem cell treatments safer.
Differentiation
Differentiation means pluripotent stem cells turn into special cells. They can become any cell from the three germ layers. This makes them very useful for science and medicine. Scientists have shown human embryonic stem cells can make all three germ layers. For example, some studies use genome-wide expression and ChIP-seq. These studies show how transcription factors like NANOG, OCT4, and SOX2 guide differentiation. These factors control genes like EOMES. EOMES starts the process for endoderm cells. EOMES works with SMAD2/3 to turn on the network for endoderm cells.
| Germ Layer | Experimental Approach | Markers Used | Key Findings |
|---|---|---|---|
| Ectoderm | Micropatterning of hPSCs to form radial patterns | PAX6 (CNS ectoderm), AP-2α (non-neural ectoderm) | hPSCs self-organize into neural and non-neural regions |
| Mesoderm | Differentiation of hPSCs into meso-endoderm, reseeded on ectoderm micropatterns | T/Brachyury (mesoderm marker) | Mesodermal cells overlap with neural ectoderm, showing selective distribution |
| Endoderm | Differentiation of hPSCs into meso-endoderm, reseeded on ectoderm micropatterns | SOX17 (endoderm marker) | Endodermal cells cluster at edges, confirming endoderm lineage |
Labs use different steps to guide differentiation. They start with good pluripotent stem cells. They coat plates, break up cell colonies, and use special media with inhibitors. Scientists watch the cells before and after they start changing. Directed differentiation uses cytokines, media, and matrices to make certain cell types. Purification steps, like sorting by surface markers, help get pure cells. Some steps are easy and work well for neural cells. Others, like for heart or liver cells, are harder and need more work. Experts work together to make these methods better. Learning how differentiation works is still very important in stem cell research.
Transcription Factors
Transcription factors are proteins that turn genes on or off. In pluripotent stem cells, some transcription factors are needed to keep their features. Oct4, Sox2, c-Myc, and Klf4 can change the cell’s epigenetic state. They swap repressive histone marks for active ones. This makes the cell pluripotent. Enzymes like histone demethylases and methyltransferases help with these changes. RNA interference screens found Esrrb and Tbx3 are needed for self-renewal. If these are blocked, the cells start to change. Nanog can stop this and keep the cells undifferentiated. Other important factors are Nac1 and Zfp281. They work with Nanog to help self-renewal.
| Transcription Factor | Role in Pluripotency Maintenance | Type of Evidence |
|---|---|---|
| Oct4 | Needed for early development and pluripotency; dosage affects lineage choice | Genetic studies |
| Sox2 | Partners with Oct4 to regulate genes; essential for pluripotency | Protein-DNA binding, functional assays |
| Nanog | Promotes self-renewal; reduces need for LIF | Functional assays |
| Sall4, Dax1, Rif1 | Support pluripotency through protein networks | Protein complex studies, RNA screens |
| Esrrb, Tbx3 | Required for self-renewal; Nanog can rescue loss | RNA interference |
| Nac1, Zfp281 | Interact with Nanog; essential for self-renewal | Protein interaction analysis |
These transcription factors work together in a network. They control which genes are active. They keep the cells undifferentiated. They also help turn regular cells into induced pluripotent stem cells. Their teamwork keeps stem cell features stable.
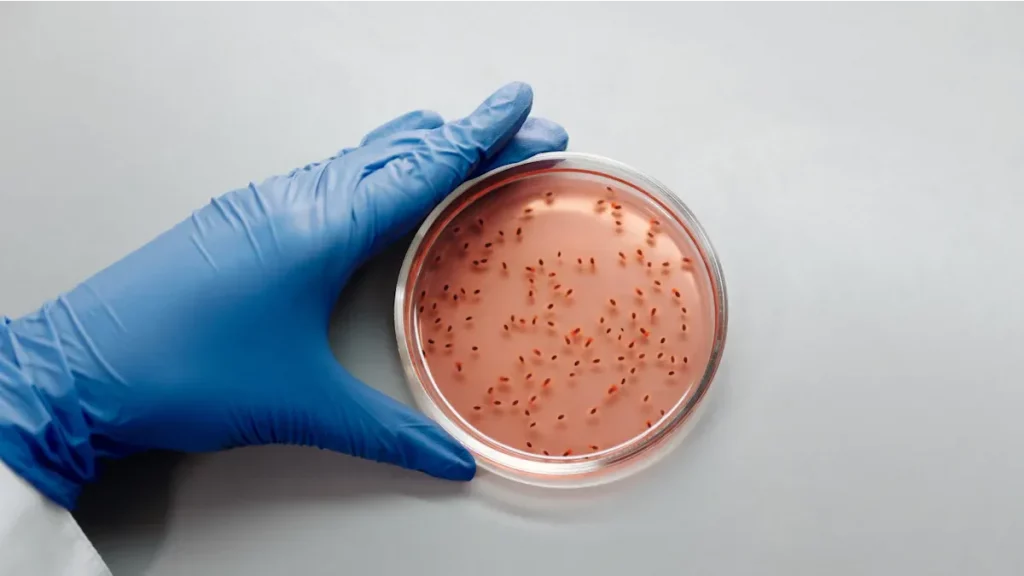
Note: Scientists use many ways to check if a cell is pluripotent. They look at the shape and structure under a microscope. They use immunophenotyping and flow cytometry to find markers like NANOG, OCT4, SSEA3/4, and TRA-1-60/81. Gene tests like qRT-PCR check for important genes. Genetic tests look for stable chromosomes. Functional tests, like embryoid body formation and directed differentiation, show if cells can become different types. Flow cytometry is a strong way to find pluripotency markers. Using all these tests gives a full view of stem cell quality and safety.
Comparison to Other Stem Cells
Totipotent
Totipotent stem cells are at the top of the stem cell family. These cells show up right after an egg and sperm join. You can find them in the zygote and early blastomeres. Totipotent cells can make every cell in the body. They also make extra tissues like the placenta and yolk sac. This makes them different from other stem cells. Both totipotent and pluripotent cells use important transcription factors. These include Oct4, Sox2, and Nanog. But totipotent cells have special markers like Zscan4 and Eomes. Their chromatin is more open. This means their DNA is easier for genes to use.
| Cell Type | Developmental Potential | Embryonic Stage |
|---|---|---|
| Totipotent | Can give rise to all cell types, including extraembryonic tissues (e.g., placenta, yolk sac) | Zygote and early blastomeres |
| Pluripotent | Can differentiate into all cell types of the three germ layers (endoderm, mesoderm, ectoderm) but cannot form extraembryonic tissues | Inner cell mass of blastocyst |
When totipotent cells change to pluripotent, their genes change too. Some genes turn off and others turn on during this switch.
Multipotent
Multipotent stem cells can only become a few types of cells. They do not have as many choices as pluripotent or totipotent cells. Multipotent stem cells are found in adults. Hematopoietic stem cells and neural stem cells are two main examples. Hematopoietic stem cells make all the blood cells. Neural stem cells make the main cells in the brain and nerves. Multipotent stem cells help fix and keep tissues healthy.
| Aspect | Pluripotent Stem Cells | Multipotent Stem Cells |
|---|---|---|
| Differentiation Capacity | Can differentiate into all cell types derived from the three germ layers (ectoderm, mesoderm, endoderm). | Can differentiate only into a limited number of cell types within a specific tissue or organ lineage. |
| Examples | Embryonic Stem Cells (ESCs), Induced Pluripotent Stem Cells (iPSCs) | Hematopoietic Stem Cells (HSCs), Mesenchymal Stem Cells (MSCs), Neural Stem Cells |
| Source | Early embryos (ESCs), reprogrammed adult cells (iPSCs) | Bone marrow, adipose tissue, umbilical cord blood |
| Clinical Use | Broad potential in regenerative medicine due to ability to generate many cell types | Used in targeted restorative therapies for specific tissues (e.g., blood, bone) |
| Potency Description | Unlimited differentiation potential within the body’s cell types | Limited differentiation potential restricted to related cell lineages |
Multipotent stem cells are the most common in adults. Scientists use hematopoietic stem cells to treat blood problems. Neural stem cells help fix the nervous system. These adult stem cells keep tissues working well as we grow older.
Unipotent
Unipotent stem cells can only make one kind of cell. For example, they might only make skin or muscle cells. These cells live in adult tissues. They help replace cells that are old or hurt. Unipotent stem cells cannot turn into other cell types. But they are still important for keeping tissues healthy. Pluripotent stem cells can become any cell in the body. Unipotent stem cells show how the body uses different stem cells for different jobs. As cells go from totipotent to pluripotent, then to multipotent and unipotent, they lose some abilities. Adult stem cells, like multipotent and unipotent, help tissues by making new cells when needed.
Note: Scientists study all these stem cell types to learn how the body grows and heals. Each type has a special job in the body and in medicine. Knowing the differences helps researchers pick the best stem cell for each treatment.
Types of Pluripotent Stem Cells

Embryonic Stem Cells
Embryonic stem cells come from the inside part of blastocysts. Scientists first found these cells in mouse embryos in 1981. In 1998, they made the first human embryonic stem cell lines. These cells can turn into almost any cell in the body. They are the best example of pluripotency.
Researchers use different ways to get embryonic stem cells:
- Mechanical dissection uses tools to pull out the inner cell mass. This way does not use animal products but takes longer.
- Laser dissection uses a laser to cut out the inner cell mass. It is very exact but costs a lot.
- Immunosurgery uses antibodies and animal serum to remove extra cells. This way is not good for clinics because it uses animal products.
After getting the cells, scientists grow them on feeder layers or special surfaces. This keeps them from changing. There are strict rules for using these cells. Donors must give consent, and ethics boards must review the research. Laws do not allow selling human eggs or embryos for research. Some states let people do this research, but others do not. Committees make sure all the rules are followed.
People argue about embryonic stem cells because of embryo status and the need for other options. Some worry about making embryos just for research. Others think the research is good for medicine.
Induced Pluripotent Stem Cells
Induced pluripotent stem cells are made by changing adult cells. Scientists use special proteins like Oct4, Sox2, c-Myc, and Klf4 to do this. They use different ways, like viruses, protein delivery, or chemicals. For example, adding Lin28-30Kc19 protein to skin cells makes 1.5 times more pluripotent colonies in one week. This makes the process work better.
Induced pluripotent stem cells may help with personal medicine. Doctors can use a person’s own cells to make new tissues. But these cells may have more genetic problems than embryonic stem cells. They might keep some features from the original adult cell. Scientists are working to make induced pluripotent stem cells safer and better for patients.
| Aspect | Induced Pluripotent Stem Cells (iPSCs) | Embryonic Stem Cells (ESCs) |
|---|---|---|
| Genetic Stability | Lower, more mutations | Higher, fewer mutations |
| Clinical Potential | Personalized therapy, safety concerns | High, ethical debates |
| Origin | Reprogrammed adult cells | Inner cell mass of embryos |
Embryonic Germ Cells
Embryonic germ cells come from primordial germ cells. These cells show up early and later become sperm or eggs. Embryonic germ cells are a lot like embryonic stem cells because they are pluripotent. But they have special epigenetic patterns because of where they come from. Germ cells erase many DNA marks, which changes what they can become.
Both embryonic germ cells and embryonic stem cells can turn into many cell types. Scientists study these cells to learn about how bodies grow and about diseases. Germ cells are also important because they pass genes to the next generation.
Applications
Research
Pluripotent stem cells are used a lot in research. Scientists use them to study diseases and how they start. iPSCs can turn into many cell types for these studies. This helps make models that show what happens in real diseases. These models let scientists test new drugs. Researchers can look at genetic diseases, like heart problems people are born with. iPSCs have the same genes as the patient. This helps scientists learn how diseases work. Animal models do not always act like humans. iPSCs help fix this problem. They can grow in big amounts, so testing is easier. Using 3D cultures and special proteins, scientists can make cells act like real tissues. These uses help with personal medicine and gene therapy. Pluripotent stem cells show promise for new treatments.
- iPSCs help model diseases like arrhythmias and other inherited problems.
- They let scientists test drugs on cells that act like human ones.
- iPSCs are used to see how cells react to different treatments.
Medicine
Pluripotent stem cells are important in regenerative medicine. They can become any cell type in the body. This helps fix or replace damaged tissues. Doctors use them to help the heart, eyes, and nerves. iPSCs come from the patient, so the body does not reject them. New ways, like non-viral reprogramming, make these cells safer. Bioengineering tools help grow tissues for transplants. Bioprinting and biomaterials can make 3D tissues and organoids. These new methods help repair tissues for many health problems.
| Disease/Condition | Stem Cell Type Used | Trial Description/Outcome | Geographic Focus |
|---|---|---|---|
| Macular degeneration | ESC-derived retinal cells | Safe transplantation in early trials | Asia (Japan) |
| Parkinson’s disease | Dopaminergic neurons from hESCs/hiPSCs | Early studies show improved protocols | Asia |
| Cardiovascular disease | ESC-derived progenitors | Promising results for heart repair | Asia |
Pluripotent stem cells could help many people in medicine. They can repair tissues better than adult stem cells. These uses show how helpful stem cell therapy can be.
Risks
Pluripotent stem cells also have some risks. One big risk is teratoma formation. If some cells do not change, they can make tumors after transplant. Even 10,000 undifferentiated cells can cause tumors in muscle. More cells mean bigger tumors. Sensitive tests can find these cells before use. Scientists use many ways to lower these risks:
- Nonintegrating gene transfer systems help avoid harmful gene changes.
- Chemical reprogramming makes the process safer.
- Only safe, fully changed cells are used for transplants.
- Suicide genes can destroy tumor cells if needed.
- Special drugs can remove undifferentiated cells.
- Pretreatment with chemicals can lower cancer risk.
- Testing in animals checks for tumors before using in people.
These steps help make stem cell treatments safer. They also help tissue repair and regeneration work better.
Pluripotent stem cells are very special for science and medicine. They can turn into almost any cell in the body. This means they are useful for studying diseases, testing new drugs, and fixing damaged tissues. When Shinya Yamanaka found iPSCs, it changed research. Scientists started looking at ways to use these cells for each patient. They also hope to grow new organs with them. Studies now focus on fixing the heart, liver, and brain. Some clinical trials look good for diseases like Parkinson’s. More companies around the world are working with these cells. The market is growing fast because people see many new uses and big chances for new discoveries.

Scientists think that if research keeps going, pluripotent stem cells will help heal and repair the body in new ways. This gives hope to people with many different diseases.
FAQ
What makes pluripotent stem cells different from other stem cells?
Pluripotent stem cells can turn into almost any cell. Multipotent stem cells can only make a few types of cells. Unipotent stem cells make just one kind of cell. Pluripotent cells give more choices for science and medicine.
Can pluripotent stem cells cure diseases?
Scientists use pluripotent stem cells to learn about diseases. They also use them to try new treatments. These cells might help fix tissues in the future. Some early studies look good, but more research is needed before most treatments are ready.
Are there risks when using pluripotent stem cells?
Yes, there are some risks. Pluripotent stem cells can make tumors called teratomas if they do not change fully. Scientists use special tests and safety steps to lower this risk before giving the cells to people.
How do scientists test if a cell is pluripotent?
Scientists look for special markers on the outside of the cell. They also check if the cells can make all three germ layers in the lab. Sometimes, they use animals to see if the cells can make many tissue types.
Where do pluripotent stem cells come from?
| Type | Source |
|---|---|
| Embryonic Stem Cells (ESCs) | Early embryos (blastocysts) |
| Induced Pluripotent Stem Cells (iPSCs) | Reprogrammed adult cells |
| Embryonic Germ Cells | Early reproductive cells |
Pingback: Blood to Potential: Chemical Reprogramming Unlocks a New Era in Regenerative Medicine - Billion Stem Cells
Pingback: Navigating the Uncharted Waters: Understanding Side Effects of Stem Cell Therapies in Humans - Billion Stem Cells