Introduction
Did you know that cardiovascular diseases (CVDs) are the leading cause of death globally, accounting for an estimated 17.9 million deaths each year? Despite advancements in medical science, current treatments for CVDs have limitations, prompting researchers to explore innovative solutions. Stem cell therapy, particularly using Mesenchymal Stem Cells (MSCs), has emerged as a promising avenue. Welcome to Billion Stem Cells, your trusted source for the latest information on stem cell technology. In this blog post, we’ll explore the latest research and clinical insights into the role of MSCs in treating cardiovascular diseases, offering hope for improved outcomes and enhanced quality of life.
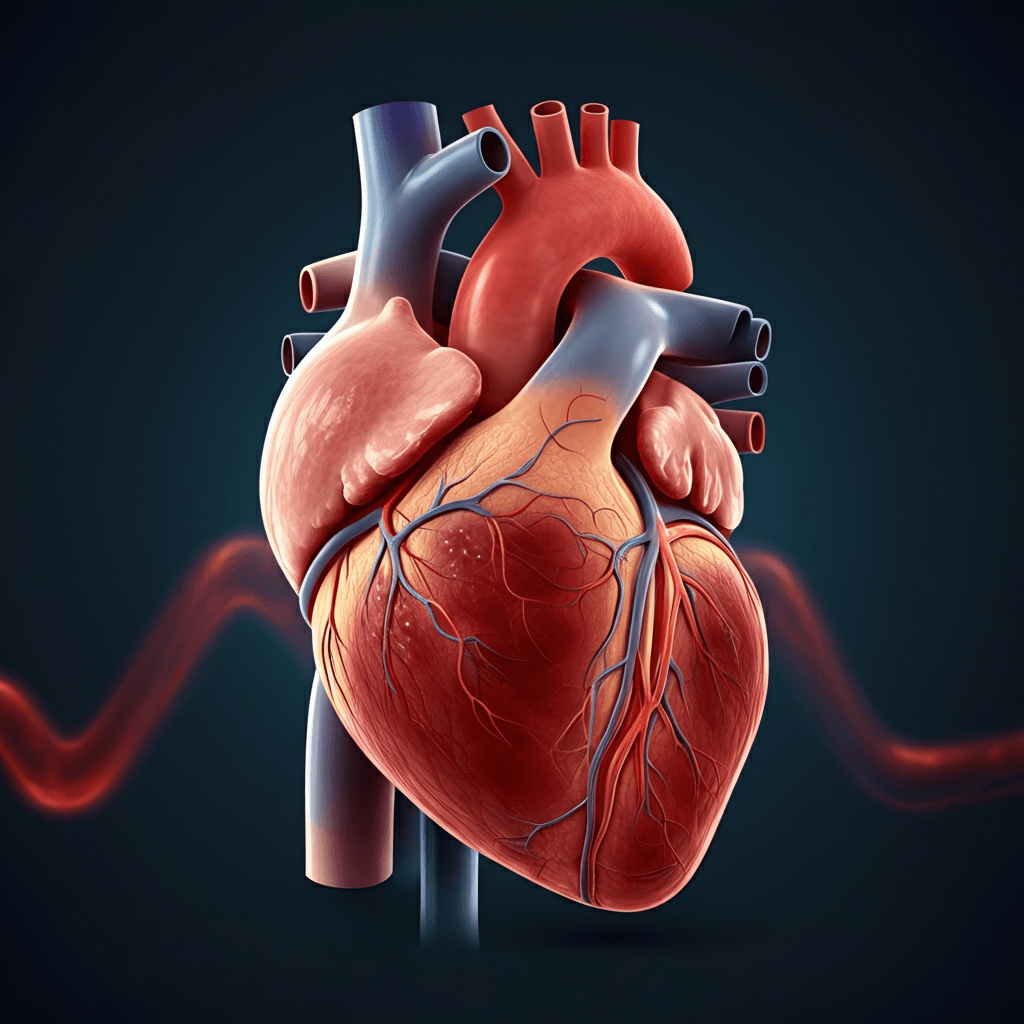
Understanding Cardiovascular Diseases (CVDs)
Cardiovascular diseases encompass a range of conditions affecting the heart and blood vessels. Common CVDs include:
- Heart Failure: A chronic condition where the heart cannot pump enough blood to meet the body’s needs.
- Coronary Artery Disease (CAD): Plaque buildup in the arteries, leading to reduced blood flow to the heart.
- Arrhythmias: Irregular heartbeats that can impair the heart’s ability to function effectively.
- Stroke: Occurs when blood supply to the brain is interrupted, leading to brain damage.
Current treatments for CVDs, such as medication, lifestyle changes, and surgical procedures, often manage symptoms but do not fully address the underlying damage. Therefore, regenerative approaches like stem cell therapy are gaining attention for their potential to repair and restore heart tissue.
What are Mesenchymal Stem Cells (MSCs)?
Mesenchymal Stem Cells (MSCs) are multipotent stromal cells that can differentiate into various cell types, including bone, cartilage, fat, and muscle cells. Key characteristics of MSCs include:
- Self-Renewal: MSCs can divide and replicate to maintain a population of stem cells.
- Differentiation: MSCs can differentiate into specialized cells to repair damaged tissues.
- Immunomodulation: MSCs can modulate the immune system, reducing inflammation and promoting tissue repair.
- Paracrine Signaling: MSCs secrete growth factors and cytokines that stimulate tissue regeneration.
MSCs can be sourced from various tissues, including:
- Bone Marrow: A traditional source of MSCs, obtained through bone marrow aspiration.
- Adipose Tissue: MSCs can be isolated from fat tissue through liposuction.
- Umbilical Cord Blood: A non-invasive source of MSCs, collected after childbirth.
How MSCs Work in Cardiovascular Repair
MSCs offer several mechanisms of action for cardiovascular repair:
- Angiogenesis: MSCs promote the formation of new blood vessels, improving blood supply to damaged heart tissue.
- Immunomodulation: MSCs regulate the immune response, reducing inflammation and preventing further damage to the heart.
- Paracrine Signaling: MSCs secrete growth factors and cytokines that stimulate the survival, proliferation, and differentiation of cardiac cells.
- Direct Differentiation: MSCs can differentiate into cardiomyocytes (heart muscle cells) and endothelial cells (cells lining blood vessels), contributing to tissue regeneration.
By promoting angiogenesis, modulating the immune system, and secreting growth factors, MSCs can effectively repair and regenerate damaged heart tissue, leading to improved cardiac function.
Latest Research on MSCs and CVDs
Recent studies and clinical trials have shown promising results regarding the use of MSCs in treating CVDs. Key findings include:
- Improved Cardiac Function: MSC therapy has been shown to improve ejection fraction (the percentage of blood pumped out of the heart with each contraction) and reduce heart failure symptoms.
- Reduced Scar Tissue: MSCs can reduce the formation of scar tissue in the heart, promoting healthier tissue regeneration.
- Enhanced Blood Flow: MSCs promote angiogenesis, leading to improved blood flow to the heart muscle.
- Decreased Inflammation: MSCs modulate the immune system, reducing inflammation and preventing further damage to the heart.
For example, a study published in the Journal of the American Heart Association found that MSC therapy significantly improved cardiac function and reduced heart failure symptoms in patients with ischemic heart disease.
MSCs Clinical Trials Heart Failure
Several clinical trials have investigated the use of MSCs in treating heart failure. Specific examples include:
- The POSEIDON Trial: This study evaluated the safety and efficacy of MSCs in patients with ischemic heart failure. Results showed that MSC therapy improved cardiac function and reduced heart failure symptoms.
- The DREAM-HF Trial: This trial investigated the use of MSCs in patients with dilated cardiomyopathy. Findings indicated that MSC therapy improved cardiac function and reduced heart failure hospitalizations.
- The ALCADIA Trial: This study evaluated the use of allogeneic (donor-derived) MSCs in patients with heart failure. Results showed that allogeneic MSC therapy was safe and effective in improving cardiac function.
Potential benefits of MSC therapy for heart failure include improved exercise capacity, reduced hospitalizations, and enhanced quality of life. However, it’s essential to consider potential risks and side effects, such as infection, immune reactions, and the possibility of tumor formation (though this is rare with MSCs).
Advantages of MSC Therapy Over Conventional Therapies
MSC therapy offers several advantages over conventional treatments for CVDs:
- Addresses Underlying Damage: Unlike medications and surgical procedures that primarily manage symptoms, MSC therapy aims to repair and regenerate damaged heart tissue.
- Potential for Long-Term Benefits: MSC therapy may provide long-term benefits by promoting tissue regeneration and improving cardiac function.
- Minimally Invasive: MSC therapy can be administered through minimally invasive procedures, reducing the risks associated with open-heart surgery.
- Personalized Treatment: MSCs can be sourced from the patient’s own body (autologous MSCs), reducing the risk of immune rejection.
By addressing the underlying damage and offering the potential for long-term benefits, MSC therapy represents a significant advancement in the treatment of CVDs.
Addressing Safety Concerns
While MSC therapy holds great promise, it’s crucial to address potential safety concerns. Key considerations include:
- Risk of Infection: As with any medical procedure, there is a risk of infection associated with MSC therapy.
- Immune Reactions: Although MSCs have immunomodulatory properties, there is a potential for immune reactions, particularly with allogeneic MSCs.
- Tumorigenicity: A common concern is whether MSCs can cause tumors. Unlike embryonic stem cells (ESCs), MSCs do not cause tumors. MSCs have a low risk of tumorigenicity because they are not pluripotent and do not have the same capacity to differentiate into any cell type in the body.
- Ectopic Tissue Formation: MSCs may differentiate into unintended cell types, leading to the formation of ectopic tissue.
To mitigate these risks, rigorous screening, quality control measures, and clinical monitoring are essential. Compared to embryonic stem cells, MSCs have a better safety profile due to their limited differentiation potential and lower risk of tumor formation.
Conclusion
In summary, MSC therapy represents a promising approach for treating cardiovascular diseases by promoting tissue regeneration, modulating the immune system, and improving cardiac function. Recent research and clinical trials have shown encouraging results, highlighting the potential of MSCs to improve outcomes and enhance the quality of life for patients with CVDs.
Future Outlook
The future of MSC therapy in CVDs is bright, with ongoing research focused on:
- Optimizing MSC Delivery: Developing more effective methods for delivering MSCs to the heart.
- Enhancing MSC Function: Improving the therapeutic potential of MSCs through genetic modification and preconditioning.
- Personalized MSC Therapy: Tailoring MSC therapy to individual patients based on their specific needs and characteristics.
Pingback: Stem Cell Therapy for Parkinson’s Disease: A Breakthrough in Regenerative Medicine - Billion Stem Cells