Donating stem cells is safer and easier in 2025. New medical advances have made it possible for more people to donate stem cells and participate in this life-saving process. Stem cell donations play a crucial role in helping patients with blood cancers live longer. For instance, three years after a transplant, 92% of Hodgkin lymphoma patients and 79% of multiple myeloma patients survive. These statistics highlight the importance of choosing to donate stem cells. By donating, you offer someone hope to heal and improve their quality of life.
Methods for Donating Stem Cells
Giving stem cells is a great way to help others. In 2025, there are two main ways to donate: peripheral blood stem cell (PBSC) donation and bone marrow donation. Each method works differently and has its own benefits. Learning about them can help you pick the best option.
Peripheral Blood Stem Cell Donation
PBSC donation is the most popular method today. It collects stem cells from your blood. Before donating, you get shots of filgrastim for a few days. This medicine helps your body make more stem cells and move them into your blood. On donation day, you sit while a machine takes stem cells from your blood. The rest of your blood goes back into your body.
Studies show this process is safe. For example, a study of over 21,000 donors found PBSC donors had fewer long-term health problems than bone marrow donors. This shows PBSC donation is both safe and helpful.
Bone Marrow Donation
Bone marrow donation is another way to give stem cells. This method takes stem cells from your bone marrow, usually from your hip bone. Unlike PBSC, this needs anesthesia. A doctor uses a needle to take the marrow. You might feel sore after, but most people recover fast.
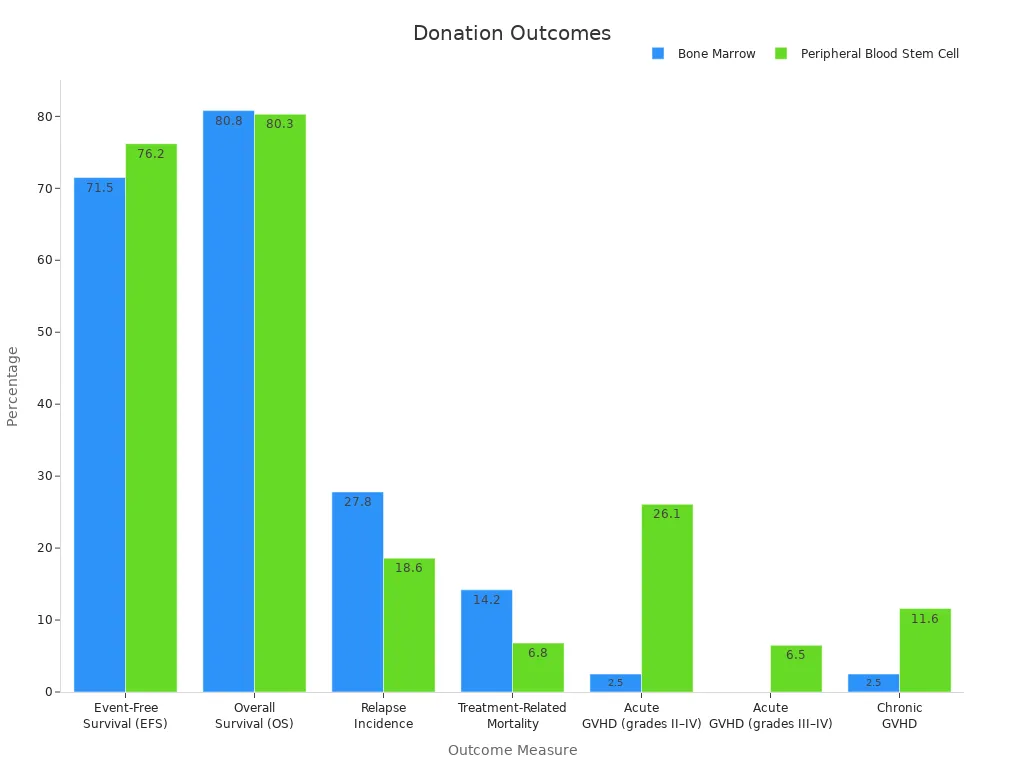
Studies show bone marrow donation is still a good option. For example, bone marrow transplants take longer to work than PBSC transplants. But they cause fewer cases of chronic graft-versus-host disease (GVHD). This makes bone marrow donation better for some patients.
| Outcome | PBSC Transplant | BMT Transplant | P-value |
|---|---|---|---|
| Neutrophil Engraftment (days) | 17 | 24 | < .001 |
| Platelet Engraftment (days) | 28 | 47 | < .001 |
| 2-Year Survival Rate | 38% | 28% | = .08 |
| Acute GVHD (Grade II-IV) | 46% | 51% | = .3 |
| Chronic GVHD (after 180 days) | Higher in PBSC | N/A | = .05 |
| Late Infections | More frequent in PBSC | N/A | N/A |
Differences Between PBSC and Bone Marrow Donation
Both methods save lives, but they are different. PBSC donation is easier and doesn’t need anesthesia. This means you recover faster. Bone marrow donation is better for some patients, like younger ones, because it lowers the risk of chronic GVHD.
Data shows these differences. PBSC transplants have higher survival rates (76.2% vs. 71.5%) and lower relapse rates (18.6% vs. 27.8%) than bone marrow transplants. But bone marrow transplants have fewer severe GVHD cases. Doctors use this information to choose the best method for each patient.
Deciding between PBSC and bone marrow donation depends on what you prefer and what the patient needs. Both are safe and can change someone’s life for the better.
Step by Step PBSC Donation Process
Screening and Eligibility Requirements
When I thought about donating blood stem cells, I found out it starts with joining the donor list. A simple cheek swab is the first step. This painless swab collects cells to check if I could match someone in need. If I matched, I’d take a blood test to confirm compatibility.
Next, I’d have a health check-up. This includes a physical exam to ensure I’m healthy enough to donate. Doctors look for any health issues that might make donating unsafe for me or the patient. The screening process is detailed but easy, keeping everyone safe.
Here’s a simple list of the steps:
- Learn, Swab, Save Lives: Join the registry with a cheek swab.
- Confirmatory Typing: Take a blood test if matched.
- Work-up: Get a physical exam to confirm you can donate.
- Donation: Give blood stem cells or bone marrow.
- Transplant: The patient receives the donated cells.
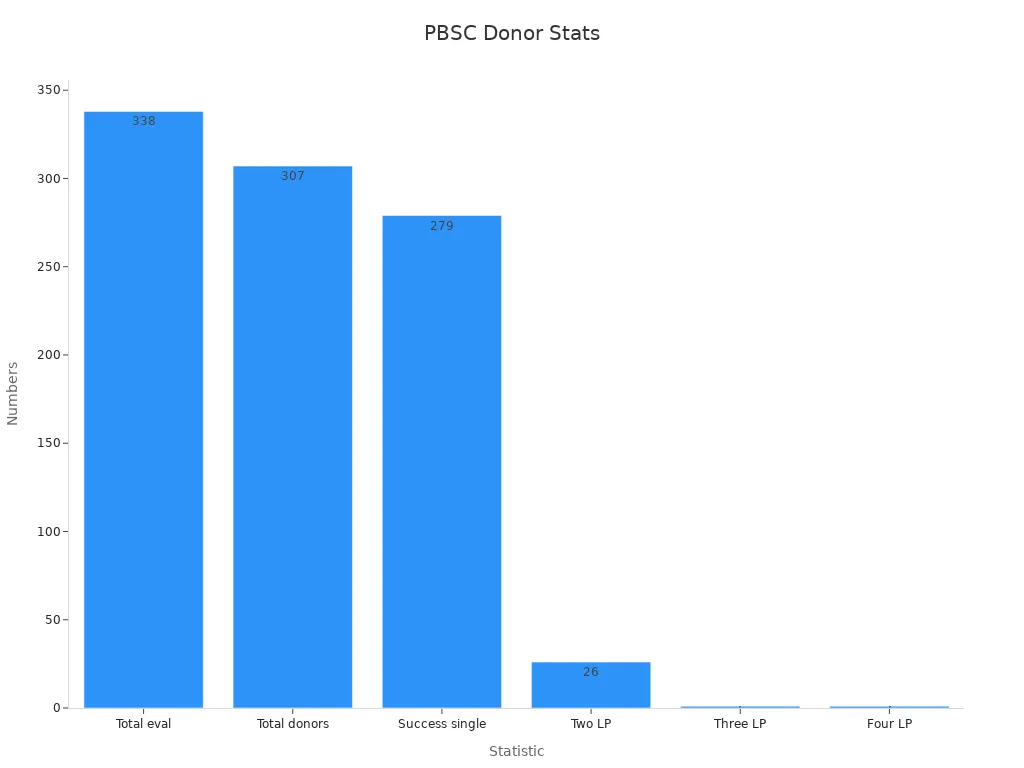
The screening success rate is high. Out of 338 collections reviewed, 307 donors were eligible. Most donors (90.9%) finished with one leukapheresis session. Only a few needed extra sessions. The average donor age was 37 years. Doctors checked health markers like hemoglobin to ensure safety.
| Statistic | Value |
|---|---|
| Total collections reviewed | 338 |
| Total eligible donors | 307 |
| Successful single leukapheresis | 279 (90.9%) |
| Donors needing two sessions | 26 (8.5%) |
| Donors needing three sessions | 1 (0.3%) |
| Donors needing four sessions | 1 (0.3%) |
What Happens on Donation Day
On donation day, I’d arrive at the clinic ready and informed. The staff would explain each step and answer my questions. Before starting, they’d do a final check-up to ensure I’m ready.
The donation process is called leukapheresis. I’d sit in a comfy chair while a machine draws blood from one arm. The machine separates blood stem cells and returns the rest of my blood through the other arm. This takes about 4 to 6 hours. During this time, I could read, watch a movie, or nap.
The staff watches donors closely during the procedure. They make sure I stay comfortable and hydrated. Knowing my donation could save a life makes it all worth it.
Recovery and Post-Donation Care
After donating, I’d rest at the clinic for a bit. The staff would give me snacks and drinks to help me recover. Most people feel normal again in a day or two. Some might feel tired or have mild bruising where the needle was.
Studies show related donors (RD) may have more lingering symptoms than unrelated donors (URD). For example, 17% of RD report not feeling fully recovered within a year, compared to 12% of URD. Still, most donors recover completely and feel proud of helping others.
To recover smoothly, I’d follow these tips:
- Drink plenty of water and eat healthy meals.
- Avoid heavy lifting or tough activities for a few days.
- Call the clinic if I notice anything unusual.
Donating blood stem cells is a powerful way to help others. By preparing and knowing what to expect, I can make the process easier for myself and the patient who benefits from my gift.
How Safe Is Stem Cell Donation?
Addressing Safety Concerns
When I thought about donating stem cells, I worried about safety. After learning more, I felt better knowing it’s well-researched. Over 30 years of studies reviewed 27,770 donations, with only 12 serious problems reported. One rare case of death from a lung clot happened, but most donors had no major issues.
| Evidence Type | Details |
|---|---|
| Study Duration | 30+ years |
| Total Donations Analyzed | 27,770 |
| Serious Adverse Events | 12 |
| Fatal Events | 1 (lung clot) |
| Most Frequent Adverse Events | Heart-related issues |
| Comparison with Peripheral Blood HSC Donors | Fewer problems reported (P < .05) |
Some risks exist but are very rare. For example, blood stem cell donors have a slightly higher chance of blood clots than bone marrow donors (7 cases vs. 1 case). Still, these risks are small, and doctors watch donors closely during the process.
Common Side Effects and Their Management
I learned that side effects are usually mild and go away quickly. Many donors feel tired, have bone pain, or get headaches. Some also feel sick, have fevers, or trouble sleeping. These symptoms often come from the medicine used to make more stem cells.
Doctors suggest rest and over-the-counter pain medicine to feel better. Drinking water and eating healthy meals also help. Female donors might face slightly higher risks, like longer hospital stays, but these are rare.
Here’s a list of common side effects donors might feel:
- Bone pain
- Tiredness
- Headaches
- Fever
- Trouble sleeping
- Feeling sick
- Skin rash
Some donors may feel sad or regretful, but most feel proud. They usually recover fully in just a few days.
Long-Term Health Impacts of Donating Stem Cells
I also wondered if donating could cause problems later. Studies show no extra health risks for donors. For example, G-CSF, the medicine used to boost stem cells, is safe for healthy people. Long-term checks, like those by the National Marrow Donor Program, show donors stay healthy even years later.
Long-term risks are very rare. Research shows no higher chance of heart problems for donors compared to others. A Swedish study found donors and non-donors had similar rates of heart issues, with no big difference in risk.
Donating stem cells is safe and carefully monitored. Knowing this made me feel confident, and I hope it helps others feel the same about this life-saving choice.
Joining the Donor Registry and Matching with a Patient
How to Sign Up for the Registry
Joining the donor registry is the first step to donate. I signed up by doing a cheek swab test. This quick and painless test collects cells to find my tissue type. The registry uses this information to match donors with patients needing stem cells. Signing up was fast, and I felt happy knowing I could help someone someday.
The National Marrow Donor Program (NMDP) runs the largest stem cell registry worldwide. It connects over 9 million U.S. donors to 42 million global donors. Expanded matching rules make it easier for patients to find matches. For example:
- Matching rates rose from 66% to 97% with mismatched donations.
- Using 5/8 matches instead of 7/8 ensures a ≥99% chance for all racial groups.
Joining the registry is easy but makes a big difference for patients waiting for help.
The Matching Process Explained
After joining the registry, I learned how matching works. Doctors compare my tissue type with patients needing transplants. They look for close matches to lower risks during the transplant. The registry uses advanced systems to make matching fast and accurate.
The U.S. needs 17.5 million bone marrow donors and 335 thousand cord blood units. Meeting these numbers could raise transplant success rates to 98.7%. Expanded matching rules help patients from different backgrounds find donors more easily.
What Happens After You’re Matched
Getting matched with a patient felt exciting and important. The registry contacted me, and I took more tests to confirm the match. Doctors explained the next steps and answered my questions. Helping someone gave me a strong sense of purpose.
Patients from diverse groups now receive transplants from mismatched or haploidentical donors. Survival rates have improved for everyone, especially recently. Disease relapse is still a challenge for recipients, but I felt proud to be part of this life-saving process.
The donation journey doesn’t stop at matching. It’s teamwork between donors, patients, and doctors. Every step matters, and being involved is truly rewarding.
Giving stem cells is a powerful way to help others. Whether you pick blood stem cell donation or bone marrow donation, it’s safe and supported. The results are amazing. For example:
- 58% of patients live 5 years after transplants.
- 53% stay disease-free, and 30% avoid major complications.
Joining the donor list is the first step to helping. By signing up, you could give someone hope and a new chance. Think about doing this incredible act. Together, we can change lives in 2025.